Abstract
Introduction: Natural killer (NK) lymphocytes are cells of innate immunity that protect against tumor and infections. NK cells recognize self and non-self HLA class I ligands, are regulated by a balance between activator and inhibitory signals through surface receptors, and can interact with HLA class I molecules on target cells. Killer-cell Immunoglobulin-like Receptors (KIRs) are inhibitory molecules expressed on NK cells and belong to the immunoglobulin superfamily. KIRs function to "educate" NK cells in effective defense against unhealthy self/non-self cells and tolerance against healthy self cells. NKs are thought to play a key role in preventing early relapse of hematologic malignancies, virus infection and graft versus host disease (GvHD) after haploidentical hematopoietic stem cell transplantation (haplo-HSCT).In B-/T-cell alpha/beta depleted haplo-HSCT, donor-versus-recipient allo-reactive NK cells can exert an efficient graft versus leukemia (GvL) effect, mediated by inhibitory KIRs where the HLA ligand is missing on recipient cells. Donor NK cells after haplo-HSCT are "immature" and not effective as the mature NKs. These immature NK cells are CD56bright, are derived from CD34+ stem cells, and mature to a CD56dim phenotype. The mature CD56dim NK cells are characterized by acquisition of KIRs, CD16 and CD57 in mature stages, which have functional significance in targeting and medicating their cytolytic activity. Based on these considerations, we performed haplo-HSCT with donor NK cell add-back to provide mature, functional immunological surveillance against tumor (MRD) and virus reactivation, which can frequently occur in manipulated haplo-HSCT for pediatric acute lymphoblastic leukemia (ALL).
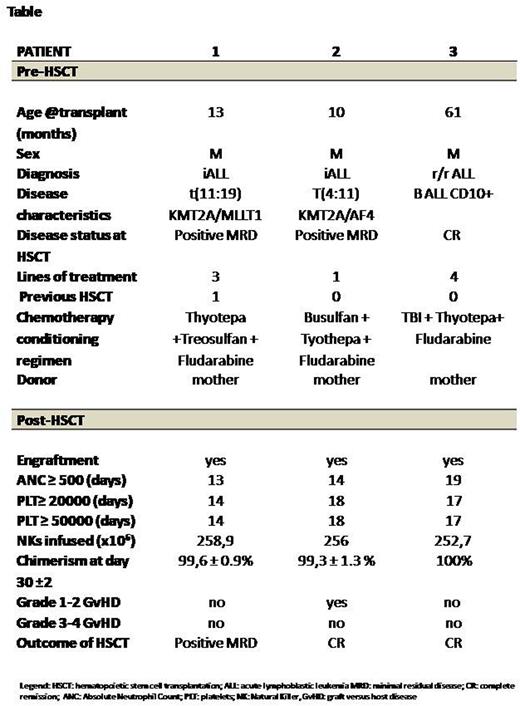
Methods: We evaluated the alloreactive effect of donor-derived NK cells in three pediatric high-risk ALL who underwent B-/T-cell alpha/beta depleted haplo-HSCT followed by donor NK infusion. Patients' characteristics are summarized in the Table. All 3 patients were male; median age was 13 months. Patients 1 and 2 had infant ALL, and patient 3 had refractory-relapsed (r/r) ALL. All patients received a median of 3 lines chemotherapy. Patient 1 received a prior allo-HSCT. Patients 1 and 2 received chemo-based conditioning regimens consisting of thyotepa, and fludarabine; In addition, patient1received treosulfan, and patient 2 received busulfan. Treosulfan was given to patient 1, due to less toxicity profile given prior allo-HSCT. Patient 3 received Total Body Irradiation (TBI), thyotepa, and fludarabine. All patients received rituximab and letermovirfor EBV and CMV prophylaxis, respectively, for all patients. Mother was Donor for all patients. Median CD34+, CD19+, CD3+-alpha/beta cell dose was 8.8, 0.05, 0.41 x 106/kg, respectively. NK cell allo-reactivity was tested by evaluating KIR genotyping and KIR/KIR-ligand mismatch in graft-versus-host direction. All three patients present KIR/KIR-ligand mismatch.
Results: Engraftment was day +13, +14 and +19 for ANC, and +14, +18 and +17 for PLT (for both >20K and >50K), for patients 1, 2 and 3, respectively. NK cell number were monitored on day +7, +14, +21 and +28 (data pending). Patients received NK cell infusion on day 30 +/- 2 days. No infusion reactions were observed. MedianNK infused were 256x106/kg. None of the patients developed CMV, EBV or ADV reactivation. Patient 2 developed Grade 2 acute GvHD (skin) treated with steroids. No Grade GvHD 3-4 was observed. Median follow up was 58 days. All patients had full donor chimerism at day 30 ±2. All patients are currently in hematological CR; patient 1 converted to positive MRD at nine months from transplant.
Conclusion: Alloreactive NK cell add-back infusion after B-/T-cell alpha/beta depleted haplo-HSCT could represent an effective option to improve transplant outcome and prevent virus reactivation. These NK cells may improve efficacy by enhancing GvL and could contribute to maintain the "disease control" through immunologic surveillance in high-risk ALL. Indeed, NK killing, which is higher in mature NK cells, depends on acquisition of sequential phenotypic maturation. Thus, infusion of mature donor NK cells may help to maintain control of MRD and virus reactivation through immunologic surveillance. Although our preliminary observations seem to be promising, this hypothesis should be confirmed in clinical trial of a larger number of patients.
Disclosures
Tambaro:Gilead: Speakers Bureau; Jazz: Other: Meeting Participation Fees, Speakers Bureau; Novartis: Other: Meeting Participation fees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal